Tracheostomy is a medical procedure that involves creating a surgical opening in the neck to provide a direct airway to the trachea. This procedure is often necessary for individuals with respiratory issues or those who require long-term mechanical ventilation. BiPAP (Bilevel Positive Airway Pressure) devices, on the other hand, are non-invasive respiratory support devices that can be crucial for managing patients with respiratory conditions. When combined, tracheostomy and BiPAP can provide effective respiratory support for patients in a home care setting. In this article, we will explore the tracheostomy procedure in detail and discuss how BiPAP devices can be utilized for home care patients.
Tracheostomy Procedure
A tracheostomy involves making an incision in the anterior part of the neck and creating a stoma (opening) directly into the trachea. This stoma allows a clear airway and enables mechanical ventilation and suctioning. The procedure is typically performed under local or general anesthesia in a hospital or surgical setting by a qualified surgeon.
During the procedure:
Tracheostomies are performed for various medical reasons, including but not limited to:
BiPAP, or Bilevel Positive Airway Pressure, is a type of non-invasive ventilation that delivers two distinct levels of pressure: one for inhalation (IPAP) and another for exhalation (EPAP). This breathing support helps patients maintain adequate oxygen levels and effectively remove carbon dioxide from their bodies. BiPAP devices are commonly used to treat various respiratory conditions, including sleep apnea, COPD, and acute respiratory failure.
BiPAP helps patients breathe more comfortably by providing a higher pressure during inhalation and a lower pressure during exhalation. This facilitates better airflow and alleviates breathing difficulties.
BiPAP devices can improve oxygenation levels in the blood, which is crucial for patients with respiratory conditions. This can lead to increased energy levels and an improved quality of life.
BiPAP machines can reduce the effort needed for breathing, making it less taxing for the patient. This can be particularly beneficial for those with weakened respiratory muscles.
BiPAP is non-invasive, meaning it does not require a surgical procedure. This is especially advantageous for home care patients who may prefer treatments that do not involve invasive interventions.
Assessment and Customization: Before initiating BiPAP therapy, a thorough assessment of the patient's respiratory needs is essential. A respiratory therapist or a healthcare provider will determine the appropriate settings for IPAP and EPAP based on the patient's condition, ensuring optimal support.
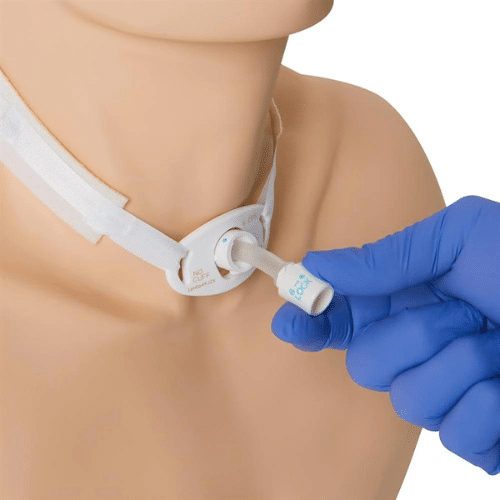
Tracheostomy Tube Selection: The choice of a tracheostomy tube is crucial when utilizing BiPAP. A tube with an appropriate size and design is chosen to ensure a secure fit and effective ventilation.
Ensuring Proper Fit and Seal: A proper fit and seal of the tracheostomy tube are crucial for the effectiveness of BiPAP therapy. Healthcare professionals ensure that the tube is securely in place and appropriately sealed to prevent air leaks.
Monitoring and Adjustment: Continuous monitoring of the patient's response to BiPAP therapy is necessary. Regular assessment of vital signs, oxygen saturation levels, and patient comfort helps in making adjustments to the BiPAP settings for optimal results.
When implementing BiPAP therapy for tracheostomized patients in a home care setting, healthcare providers need to consider various factors to ensure the safety, effectiveness, and comfort of the patient. Here are some critical considerations:
Training and Education: Proper training and education for both the patient and their caregivers are essential. This includes understanding the proper use of the BiPAP device, recognizing signs of complications, and knowing how to troubleshoot common issues.
Careful Monitoring: Regular monitoring of the patient's vital signs, respiratory status, and comfort levels is crucial. Healthcare professionals should ensure that the BiPAP settings are appropriate and effective for the patient's needs.
Maintaining Airway Hygiene: Tracheostomy care is paramount to prevent infections and ensure the stoma remains clean and free of obstructions. Proper cleaning and maintenance of the tracheostomy tube and surrounding area are vital.
Emergency Preparedness: Home care providers should equip patients and caregivers with information on what to do in case of emergencies.
Equipment Maintenance: Regular maintenance and cleaning of the BiPAP device and its accessories are essential to ensure optimal performance and prevent infections.
Collaborative Care: Effective communication and collaboration among healthcare providers, including physicians, nurses, respiratory therapists, and home care agencies, are crucial to providing comprehensive and coordinated care for the patient.
The use of BiPAP devices for tracheostomized patients in a home care setting offers significant benefits in managing respiratory issues. However, careful consideration of various factors, including proper training, monitoring, maintenance, and emergency preparedness, is essential. This ensures safe and effective BiPAP therapy for tracheostomized patients receiving home care. Working collaboratively with healthcare professionals will help optimize the use of BiPAP devices in this patient population.